Does Medicaid Cover Braces? Powerful Tips to Get Approved Faster

Does Medicaid Cover Braces? Everything You Need to Know About Medicaid and Orthodontics
Background: What You Need to Know about Medicaid and Orthodontics
If you or your children are looking into braces to correct your dental issues, one question you may be asking is, “Does Medicaid cover braces? Medicaid is the government program that offers health insurance to low-income people and families, though it covers somewhat different services in each state. Though Medicaid typically includes basic health care services, orthodontic treatments, such as braces, may not be covered by all plans.
In this detailed guide, we will break down the nuts and bolts of Medicaid’s coverage of braces, like who is eligible for this coverage, what sort of braces Medicaid might cover, and how you can get through the process of getting braces for you or your child. If you stick around until the end of this post, you’ll know exactly what Medicaid braces coverage looks like and what you have to work with.
What is Medicaid?

Medicaid is a state and federal program for low-income individuals and families with few assets. It is run by the states, so there are different rules and eligibility requirements for every state. That means that what Medicaid pays for can vary widely depending on which state you call home.
Medicaid is designed to cover a wide array of health services, including doctor visits, hospital care, prescription drugs and, in some states, dental. Some Medicaid programs cover the braces and other orthodontics, while others do not.
Does Medicaid Cover Braces? The Basics
To determine whether Medicaid pays for braces? though, it’s worth noting that Medicaid does provide orthodontic coverage in certain cases. The general rule is that Medicaid will cover braces if they are medically necessary. In other words, if braces are required to treat a health condition such as severe malocclusion (improper alignment of the teeth) or other health issues related to dental problems that could negatively affect your overall well-being, then Medicaid would cover the cost of braces.
Medicaid and Braces for Children
Medicaid is more likely to cover braces for kids younger than 21 if they have certain medical problems. Braces on Kids are Usually an Option if it cures of the following SituationBraces for KidsWhen are braces for kids an option?
- Significant bite issues (underbite, overbite, crossbite)
- When the teeth are too crowded and it’s hard to chew, speak, and clean the teeth.
- Jaw problems that affect mouth and jaw movements
In which cases, Medicaid will usually provide coverage for braces if they are needed to address these kind of medical issues. It will depend on how severe the condition is and what the likely benefits of getting braces are in whether Medicaid authorizes paying for them.
Adult Braces and Medicaid

Among adults, coverage for braces is more limited. Unless it is medically necessary to correct a medical problem, Medicaid will not pay for orthodontic work for adults in most states. However, NEMT may be available on a limited basis to adults in some states in some circumstances, including:
Post-surgical orthodontics after jaw surgery
- Jaw misalignment that results in pain, or other medical condition.
In general, Medicaid does not cover braces for purely cosmetic purposes for adults. If you’re an adult who’s considering braces, and who doesn’t qualify for braces on the basis of medical necessity and Medicaid’s standards, you may need to look to other alternatives, like private insurance or financing.
How to Tell if Braces are Covered by Medicaid
Whether or not Medicaid covers braces is all about the Medicaid plan that you are enrolled in, and maybe the state that you live in. Here is where you will find out how to tell if you can get braces with Medicaid:
Check Your State’s Medicaid Guidelines
Not at this time since Medicaid is state funded all states have different rules or regulations regarding orthodontic treatment. You can begin by checking your state’s Medicaid policy and seeing if they cover braces under your particular plan.
You may want to visit your state’s Medicaid site or reach out to your local Medicaid office to find more information on coverage, the qualifications, and possibly any limitations, of orthodontic treatment.
Determine Medical Necessity
Usually, Medicaid will cover braces only if they are medically necessary. Braces also should be medically necessary, such as to address a severe bite problem, jaw misalignment, or teeth crowding. Braces typically will not be covered by medicaid for cosmetic reasons, or for mild cases.
You will need documentation from your orthodontist or dentist to verify that your braces are medically necessary. The orthodontist should carefully examine your teeth and jaw, and possibly x-rays or other diagnostic tools need to be used to determine the extent of the problem.
Seek Prior Authorization
The program known as Medicaid often requires prior authorization before it will cover braces. This means you will have to first apply to Medicaid and prove that the treatment is medically necessary in order to receive any kind of orthodontic treatment.
If you are approved by Medicaid, they will send you specifics on your coverage and how much of the treatment will be paid for by them. Note that Medicaid may or may not approve coverage for some of the treatment but not all of the cost, depending on the rules in your state and your particular circumstances.
What Types of Braces Does Medicaid Cover
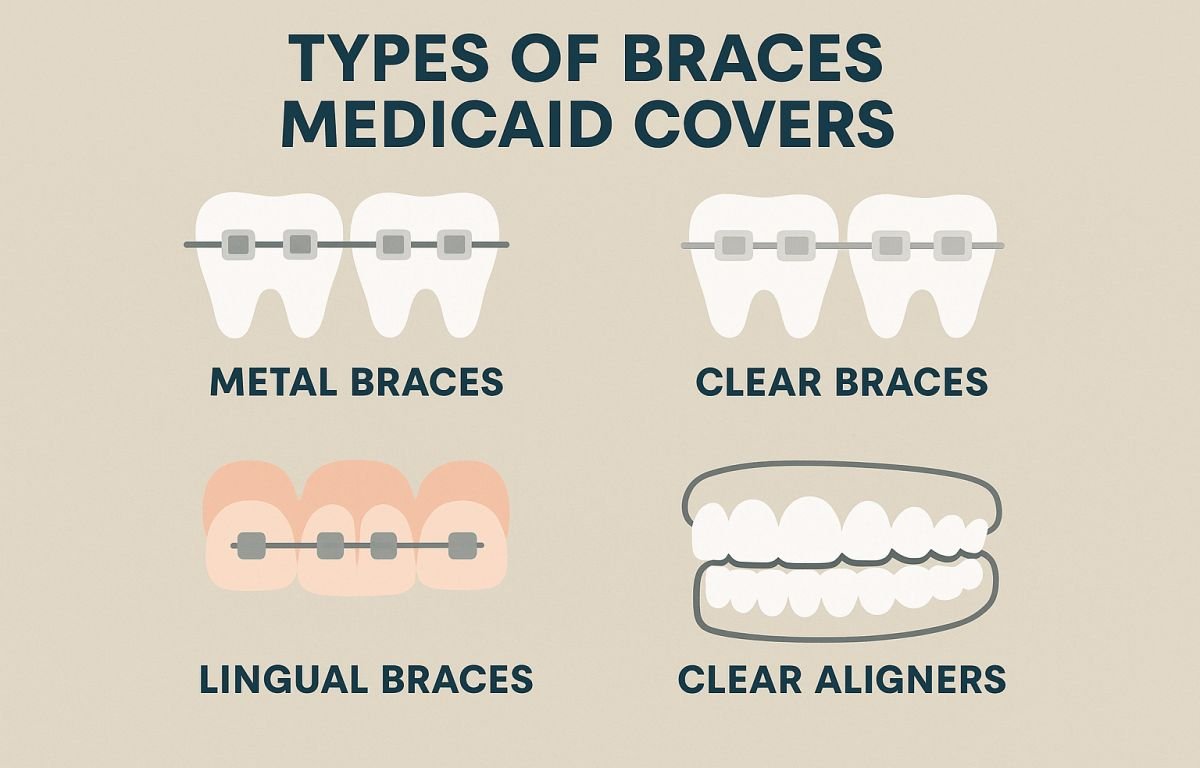
If you are then eligible, the question is, “Does Medicaid pay for braces, and if so, which type?” This depends on your state’s Medicaid program and the details of your treatment plan and is not a quick yes or no.
Metal Braces
The most common type of braces, made of high-grade stainless steel. They’re made up of metal brackets and wires that shift your teeth into the right position. When they’re medically necessary, metal braces are the type of braces Medicaid is most likely to cover.
Cost: Metal braces are the cheapest choice and tend to be the most cost-effective for Medicaid to cover.
Factors to consider: In general, Medicaid will be more likely to approve metal braces rather than something that is more cosmetic looking, unless it’s for a special medical condition.
Ceramic Braces
Ceramic braces function like metal braces, they are just clear or tooth-colored. Although these braces are less visible, they tend to be more costly than traditional metal braces.
Cost: Ceramic braces are generally more expensive, and your Medicaid may only pay for them if they are deemed medically necessary. In other states, Medicaid will only cover ceramic brackets if metal brackets are not appropriate.
Notes: Ceramic braces… Medicaid Coverage for Ceramic Braces Read More »
Clear Aligners (Invisalign)
Newly available on the market are removable braces known as clear aligners (eg Invisalign). They are clear and removable, so it is one of the most favoured option for those who want a less noticeable treatment. But generally, clear aligners cost more than metal braces and are not typically covered by Medicaid.
Expense: Clear aligners can be very costly in comparison to metal braces. Just about no insurer besides Medicaid pays for clear aligners except in cases when they are considered medically needed — such as when other treatments are inappropriate.
Considerations: Medicaid probably won’t pay for clear aligners in most cases, although you can check with your state Medicaid program to be sure.
Medicaid and Braces For Kids

One of the more frequent uses of Medicaid benefits is for children who require orthodontic work. Because the benefits of orthodontic treatment are consider less if you get it in adulthood rather than during childhood or adolescence, children may be eligible for Medicaid if they are proven to have a medical need. But children’s coverage rules may also be different from state to state, and not all dental conditions are as severe.
Severe Bite Problems
Kids who have extreme bite issues like overbites, underbites, and crossbites have a better chance of getting Medicaid to approve coverage for braces. These concerns may have an impact on the aesthetic and functional aspects of a child’s teeth so it is important to undergo orthodontic intervention for the entire health of the mouth.
Crowded Teeth
Overcrowded teeth that create obstacles to a child being able to keep good oral hygiene might also qualify for Medicaid support. Braces can straighten the teeth, enabling you to brush and floss the teeth properly, to decrease the risk for cavities and gum disease.
Jaw Alignment Issues
Medicaid could accept children who have severe malocclusion as a candidate for braces. They can affect chewing and the look of the smile.
Best Teeth Braces Colors for Every Skin Tone – Pick Your Perfect Match!
How to Get Medicaid Coverage for Braces
If your child or you need braces, and you think Medicaid might cover the cost, take these steps to apply:
Talk to your Orthodontist: Begin with a discussion with your orthodontist to check whether you even need braces. Your orthodontist can thoroughly examine and diagnose the condition that needs treatment.
Send Documentation: Send doctors prescription and cast impression along with your medicaid card for proof of eligibility to Medicaid. This could involve x-rays, photographs and a report from the orthodontist regarding the treatment proposed.
Request Prior Authorization: Before Medicaid will cover braces, they will usually require prior authorization. Make sure your request is delivered far in advance of when any treatment is required.
Await Approval: After Medicaid receives the application, they will examine the records to determine if the coverage is approved. If things go through, they’ll give you coverage information and how much it’ll cost.
Conclusion: Does Medicaid Cover Braces?
So, does Medicaid cover braces? is yes, but only in certain cases when braces will be considered necessary for health reasons. Medicaid generally pays for orthodontic work for kids under the age of 21, especially when braces are medically necessary to fix serious dental problems such as bite issues, jaw alignment problems, or overcrowded teeth. When it comes to braces for adults, though, the type of Medicaid coverage is limited — most likely, they need to be medically necessary to be considered for coverage.
If you think you or your child might be eligible for Medicaid to pay for braces, be sure to contact the Medicaid director in your state to find out what it covers. Working with an orthodontist and submitting all required documentation also increases chances of getting approval for treatment.
If you study the rules and work the process wisely, you can see to it that your orthodontic needs are met, all while taking advantage of Medicaid to lower the costs of braces.
